by John R. Lee, M.D. and Virginia Hopkins
Q: What is progesterone?
A: Progesterone is a steroid hormone made by the corpus luteum of the ovary at ovulation, and in smaller amounts by the adrenal glands. Progesterone is manufactured in the body from the steroid hormone pregnenolone, and is a precursor to most of the other steroid hormones, including cortisol, androstenedione, the estrogens and testosterone.
In a normally cycling female, the corpus luteum produces 20 to 30 mg of progesterone daily during the luteal phase of the menstrual cycle.
Q: Why do women need progesterone?
A: Progesterone is needed in hormone replacement therapy for menopausal women for many reasons, but one of its most important roles is to balance or oppose the effects of estrogen. Unopposed estrogen creates a strong risk for breast cancer and reproductive cancers.
Estrogen levels drop only 40-60% at menopause, which is just enough to stop the menstrual cycle. But progesterone levels may drop to near zero in some women. Because progesterone is the precursor to so many other steroid hormones, its use can greatly enhance overall hormone balance after menopause. Progesterone also stimulates bone-building and thus helps protect against osteoporosis.
Q: Why not just use the progestin Provera as prescribed by most doctors?
A: Progesterone is preferable to the synthetic progestins such as Provera, because it is natural to the body and has no undesirable side effects when used as directed.
If you have any doubts about how different progesterone is from the progestins, remember that the placenta produces 300-400 mg of progesterone daily during the last few months of pregnancy, so we know that such levels are safe for the developing baby. But progestins, even at fractions of this dose, can cause birth defects. The progestins also cause many other side effects, including partial loss of vision, breast cancer in test dogs, an increased risk of strokes, fluid retention, migraine headaches, asthma, cardiac irregularities and depression.
Q: What is estrogen dominance?
A: Dr. Lee has coined the term “estrogen dominance,” to describe what happens when the normal ratio or balance of estrogen to progesterone is changed by excess estrogen or inadequate progesterone. Estrogen is a potent and potentially dangerous hormone when not balanced by adequate progesterone.
Both women who have suffered from PMS and women who have suffered from menopausal symptoms, will recognize the hallmark symptoms of estrogen dominance: weight gain, bloating, mood swings, irritability, tender breasts, headaches, fatigue, depression, hypoglycemia, uterine fibroids, endometriosis, and fibrocystic breasts. Estrogen dominance is known to cause and/or contribute to cancer of the breast, ovary, endometrium (uterus), and prostate.
Q: Why would a premenopausal woman need progesterone cream?
A: In the ten to fifteen years before menopause, many women regularly have anovulatory cycles in which they make enough estrogen to create menstruation, but they don’t make any progesterone, thus setting the stage for estrogen dominance. Using progesterone cream during anovulatory months can help prevent the symptoms of PMS.
We now know that PMS can occur despite normal progesterone levels when stress is present. Stress increases cortisol production; cortisol blockades (or competes for) progesterone receptors. Additional progesterone is required to overcome this blockade, and stress management is important.
Q: What is progesterone made from?
A: The USP progesterone used for hormone replacement comes from plant fats and oils, usually a substance called diosgenin which is extracted from a very specific type of wild yam that grows in Mexico, or from soybeans. In the laboratory diosgenin is chemically synthesized into real human progesterone. The other human steroid hormones, including estrogen, testosterone, progesterone and the cortisones are also nearly always synthesized from diosgenin.
Some companies are trying to sell diosgenin, which they label “wild yam extract” as a medicine or supplement, claiming that the body will then convert it into hormones as needed. While we know this can be done in the laboratory, there is no evidence that this conversion takes place in the human body.
Q: Where should I put the progesterone cream?
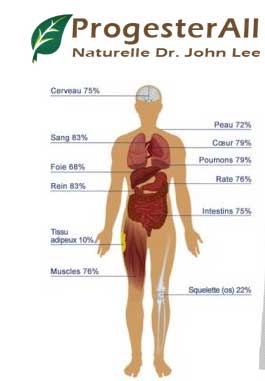
A: Because progesterone is very fat-soluble, it is easily absorbed through the skin. From subcutaneous fat, progesterone is absorbed into capillary blood. Thus absorption is best at all the skin sites where people blush: face, neck, chest, breasts, inner arms and palms of the hands.
Q: What is the recommended dosage of progesterone?
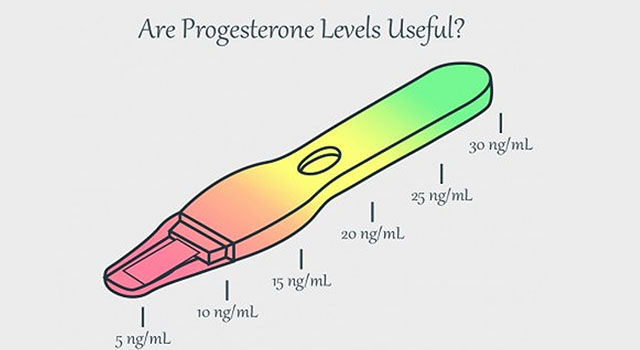
A: For premenopausal women the usual dose is 15-24 mg/day for 14 days before expected menses, stopping the day or so before menses.
For postmenopausal women, the dose that often works well is 15 mg/day for 25 days of the calendar month.
Q: What amount of progesterone do you recommend in a cream?
A: Dr. Lee recommends the creams that contain 450-500 mg of progesterone per ounce, which is 1.6% by weight or 3% by volume. This means that about one quarter teaspoon daily would provide about 20 mg/day.
Q: How safe is progesterone cream?
A: During the third trimester of pregnancy, the placenta produces about 300 mg of progesterone daily, so we know that a one-time overdose of the cream is virtually impossible. If you used a whole jar at once it might make you sleepy. However, Dr. Lee recommends that women avoid using higher than the recommended dosage to avoid hormone imbalances. More is not better when it comes to hormone balance.
Q: Wouldn’t it be easier to just take a progesterone pill?
A: Dr. Lee recommends the trans dermal cream rather than oral progesterone, because some 80% to 90% of the oral dose is lost through the liver. Thus, at least 200 to 400 mg daily is needed orally to achieve a physiologic dose of 15 to 24 mg daily. Such high doses create undesirable metabolites and unnecessarily overload the liver.
Q: Where can I get more information on progesterone and natural hormone balance?
A: For a detailed explanation of women’s hormone balance issues, a hormone balance program, as well as detailed descriptions of how to use natural progesterone, the following books by John R. Lee, M.D. are recommended:
What Your Doctor May Not Tell You About Menopause
What Your Doctor May Not Tell You About PREmenopause
What Your Doctor May Not Tell You About Breast Cancer

Q: Qu’est-ce que la progestérone?
R: La progestérone est une hormone stéroïde fabriquée par le corps jaune de l’ovaire lors de l’ovulation et, en moindre quantité, par les glandes surrénales. La progestérone est fabriquée dans le corps à partir de la prégnénolone, une hormone stéroïde, et est un précurseur de la plupart des autres hormones stéroïdes, notamment le cortisol, l’androstènedione, les œstrogènes et la testostérone.
Chez une femme à cycle normal, le corps jaune produit 20 à 30 mg de progestérone par jour pendant la phase lutéale du cycle menstruel.
Q: Pourquoi les femmes ont-elles besoin de progestérone?
R: La progestérone est nécessaire dans le traitement hormonal substitutif chez les femmes ménopausées pour de nombreuses raisons, mais l’un de ses rôles les plus importants consiste à équilibrer ou à contrecarrer les effets de l’œstrogène. L’œstrogène non opposé crée un risque élevé de cancer du sein et de cancer de la reproduction.
Les niveaux d’œstrogène ne chutent que de 40 à 60% à la ménopause, ce qui est juste assez pour arrêter le cycle menstruel. Mais les niveaux de progestérone peuvent chuter à près de zéro chez certaines femmes. Parce que la progestérone est le précurseur de nombreuses autres hormones stéroïdiennes, son utilisation peut considérablement améliorer l’équilibre hormonal après la ménopause. La progestérone stimule également la formation d’os et contribue ainsi à protéger contre l’ostéoporose.
Q: Pourquoi ne pas simplement utiliser le progestatif Provera tel que prescrit par la plupart des médecins?
R: La progestérone est préférable aux progestatifs synthétiques tels que Provera, car elle est naturelle pour le corps et ne présente aucun effet secondaire indésirable si elle est utilisée conformément aux instructions.
Si vous avez des doutes sur la différence entre la progestérone et les progestatifs, rappelez-vous que le placenta produit 300 à 400 mg de progestérone par jour au cours des derniers mois de la grossesse, nous savons que de tels niveaux sont sans danger pour le bébé en développement. Mais les progestatifs, même à des fractions de cette dose, peuvent causer des anomalies congénitales. Les progestatifs entraînent également de nombreux autres effets indésirables, notamment une perte partielle de la vision, le cancer du sein chez les chiens d’essai, un risque accru d’AVC, une rétention hydrique, des migraines, un asthme, des irrégularités cardiaques et une dépression.
Q: Qu’est-ce que la dominance en œstrogènes?
R: Le Dr Lee a inventé le terme “dominance en œstrogènes” pour décrire ce qui se produit lorsque le rapport normal ou le rapport normal entre l’œstrogène et la progestérone est modifié par un excès d’œstrogène ou une progestérone insuffisante. Les œstrogènes sont une hormone puissante et potentiellement dangereuse lorsqu’ils ne sont pas équilibrés par une progestérone adéquate.
Les femmes atteintes du syndrome prémenstruel et les symptômes ménopausiques reconnaîtront les symptômes caractéristiques de la dominance œstrogénique: prise de poids, ballonnements, sautes d’humeur, irritabilité, seins douloureux, maux de tête, fatigue, dépression, hypoglycémie, fibromes utérins, endométriose. et seins fibrokystiques. La dominance en œstrogènes est connue pour causer et / ou contribuer au cancer du sein, des ovaires, de l’endomètre (utérus) et de la prostate.
Q: Pourquoi une femme non ménopausée aurait-elle besoin d’une crème à la progestérone?
R: Au cours des dix à quinze années précédant la ménopause, de nombreuses femmes subissent régulièrement des cycles anovulatoires au cours desquelles elles produisent suffisamment d’oestrogènes pour créer la menstruation, mais elles ne produisent pas de progestérone, ce qui ouvre la voie à une dominance d’oestrogène. L’utilisation d’une crème à la progestérone pendant les mois anovulatoires peut aider à prévenir les symptômes du SPM.
Nous savons maintenant que le syndrome prémenstruel peut survenir malgré des niveaux normaux de progestérone en présence de stress. Le stress augmente la production de cortisol; le cortisol bloque (ou est en compétition pour) les récepteurs de la progestérone. Un supplément de progestérone est nécessaire pour surmonter ce blocage et la gestion du stress est importante.
Q: De quoi est faite la progestérone?
R: La progestérone USP utilisée pour le remplacement des hormones provient de graisses et d’huiles végétales, généralement une substance appelée diosgénine, extraite d’un type très spécifique d’igname sauvage poussant au Mexique ou de soja. En laboratoire, la diosgénine est synthétisée chimiquement en progestérone humaine réelle. Les autres hormones stéroïdes humaines, notamment les œstrogènes, la testostérone, la progestérone et les cortisones, sont également presque toujours synthétisées à partir de diosgénine.
Certaines entreprises essaient de vendre de la diosgénine, qu’elles qualifient d’extrait d’igname sauvage, en tant que médicament ou complément, affirmant que le corps le convertira ensuite en hormones, si nécessaire. Bien que nous sachions que cela peut être fait en laboratoire, rien ne prouve que cette conversion ait lieu dans le corps humain.
Q: Où devrais-je mettre la crème à la progestérone?
R: La progestérone étant très liposoluble, elle est facilement absorbée par la peau. De la graisse sous-cutanée, la progestérone est absorbée dans le sang capillaire. Ainsi, l’absorption est optimale sur tous les sites cutanés où les gens rougissent: visage, cou, poitrine, seins, intérieur des bras et paumes des mains.
Q: Quelle est la posologie recommandée de progestérone?
R: Pour les femmes non ménopausées, la dose habituelle est de 15 à 24 mg / jour pendant 14 jours avant la menstruation prévue, le jour ou la fin précédant les règles.
Pour les femmes ménopausées, la dose qui fonctionne souvent bien est de 15 mg / jour pendant 25 jours du mois civil.
Q: Quelle quantité de progestérone recommandez-vous dans une crème?
R: Le Dr Lee recommande les crèmes contenant de 450 à 500 mg de progestérone par once, ce qui représente 1,6% en poids ou 3% en volume. Cela signifie qu’environ un quart de cuillère à thé par jour fournirait environ 20 mg / jour.
Q: Quel est le degré de sécurité de la crème à la progestérone?
R: Au cours du troisième trimestre de la grossesse, le placenta produit environ 300 mg de progestérone par jour. Nous savons donc qu’un surdosage unique de crème est pratiquement impossible. Si vous utilisiez un pot entier à la fois, cela pourrait vous rendre somnolent. Cependant, le Dr Lee recommande aux femmes d’éviter d’utiliser une dose supérieure à celle recommandée pour éviter les déséquilibres hormonaux. Plus n’est pas meilleur quand il s’agit d’équilibre hormonal.
Q: Ne serait-il pas plus simple de prendre un comprimé de progestérone?
R: Le Dr Lee recommande la crème trans dermique plutôt que la progestérone orale, car environ 80% à 90% de la dose orale est perdue par le foie. Ainsi, au moins 200 à 400 mg par jour sont nécessaires par voie orale pour atteindre une dose physiologique de 15 à 24 mg par jour. De telles doses créent des métabolites indésirables et surchargent inutilement le foie.
Q: Où puis-je obtenir plus d’informations sur la progestérone et l’équilibre hormonal naturel?
R: Pour une explication détaillée des problèmes d’équilibre hormonal chez les femmes, un programme d’équilibre hormonal, ainsi que des descriptions détaillées sur l’utilisation de la progestérone naturelle, les ouvrages suivants de John R. Lee, M.D. sont recommandés:
Ce que votre médecin ne peut pas vous dire à propos de la ménopause
Ce que votre médecin ne peut pas vous dire à propos de la pré-ménopause
Ce que votre médecin peut ne pas vous dire à propos du cancer du sein
Progesterone Wikipedia , La cream progesterone , Cream progesterone , Progesterone France , progesterall cream , Progesterone naturelle micronizer , Progeterall john lee , La progesterone naturelle , Équilibre hormonal , Hormones , Hormone naturelle